Balance Error Scoring System with force/pressure platform
- Cláudia Tonelo

- 11 oct 2021
- 5 Min. de lectura
A look at the Balance Error Scoring System with force/pressure platform
The Balance Error Scoring System (BESS) is a well-known tool to evaluate the effects of a head injury on static postural stability, or standing still in different positions. This protocol is often used in athletes after sport-related concussions or mild traumatic brain injuries (TBIs) [1].
BESS was developed by researchers and clinicians at the University of North Carolina Sports Medicine Research Laboratory in Chapel Hill, so as to provide a quick and efficient tool for balance assessment, that could help health professionals in making return to play decisions after mild head injury. It is also part of the Sport Concussion Assessment Tool (SCAT), which is a standardized tool for evaluating a suspected concussion.
PhysioSensing Balance Software has an improved version of the traditional BESS test. In a traditional BESS test, scoring is time and error based, using a stopwatch and counting the number of occurred errors. With PhysioSensing’s solution, time and error counting is enhanced with an objective quantification of sway.
How is it done?
This protocol measures the postural stability in six conditions:
1. Two feet together on firm surface;
2. One leg standing (non-dominant foot) on firm surface;
3. Tandem position (non-dominant foot behind the other) on firm surface;
4. Two feet together on foam surface;
5. One leg standing (non-dominant foot) on foam surface;
6. Tandem position (non-dominant foot behind the other) on foam surface.
Figure 1 – Interface for BESS protocol for two feet together, one leg standing and tandem position.
The patient must maintain the position for 20 seconds with eyes closed and hands on hips. During each test, the number of errors can be added in the protocol interface. By error it is understood:
1) Remove the hands from the iliac crests;
2) Taking steps, stumbling or falling;
3) Move too much the hips;
4) Lift the front of the foot or the heel;
5) Stay out of position for more than 5 seconds.
The maximum number of errors for a single condition is 10. If multiple errors occur at the same time, only one is counted. Total error score can be 0 up to 60, and a higher score indicates poor performance.
Measures calculated
After performing all the conditions of the protocol, the values of the Sway Index and Sway Velocity for each of the conditions appear. The sway index is the variation of the distance travelled of the COP from the average position during the test time. While sway velocity is the displacement of the center of pressure during the trial divided by the time (°/s). Both concepts can be observed in Figure 2, in which the circles on the statokinesigram represent the sway index (the higher the sway index the more unsteady the person was during the test), and the right side illustrates the variation of COP (sway displacement) during each acquisition (100 acquisitions per second), allowing the calculation of the COP sway velocity in degree per second.

Figure 2 - The body sway can be translated into center of pressure values in the mediolateral and anteroposterior directions (statokinesigram), and the software posteriorly analyzes the COP displacement (ΔDn) during the trial to calculate the sway index and the mean COP sway velocity (°/s).
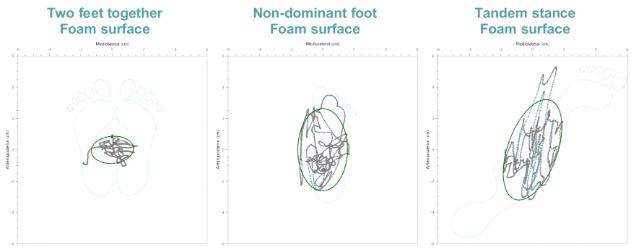
The software also provides the ellipse area containing 95% of the COP values. In addition, the center of pressure trace for each condition as well as the representation of the calculated ellipse can be observed (Figure 3).
Figure 3 – Example of the results section table and COP trace with ellipse representation for the foam surface conditions.
All this information can be quickly exported to a PDF report, and also view the progress between evaluations. This allows a more objective and quantitative look at the postural stability measurements in addition to the traditional error counting.
Significance
There is no normative data for this enhanced version of the BESS test. However, there are several studies aimed to provide normative information using the traditional BESS, for example, Grant L. Iverson et al. administered BESS in 589 healthy community-dwelling adults so as to facilitate interpretation of BESS performance in patients with traumatic brain injuries or other neurological conditions [2].
Nevertheless, there are several considerations that can be established from the results on each condition of BESS using force/pressure platforms:
Healthy individuals show minimal sway on the firm surface with feet together. On the other hand, sway increases on non-dominant foot and tandem position, mainly with foam surface. Even healthy individuals may lose balance or fall on those four conditions;
High values of sway velocity with feet together on firm surface should be interpreted with caution, as this condition is the same as the Romberg test, which showed to be insensitive to changes in postural sway after mild injury [3];
In the case of high values in the non-dominant foot and/or tandem position on firm surface, it is indicative of ankle instability (mainly mediolateral in the tandem stance), problems with sensory integration or inability to generate a more effective counterbalance strategy due to orthopedic limitations or pain [4]-[5].
For the last 3 conditions (foam surface conditions), high values are indicative of sensory integration problems, however biomechanical factors should not be completely excluded. Even healthy individuals can lose their balance in those conditions, in which vestibular information must be used to control the balance [6].
In addition, according to the systematic review from David R. Bell et al., BESS shows moderate to good reliability for static balance assessment, and can detect balance problems in individuals with concussion and fatigue [1]. Regarding instrumented BESS with force plate, it has also shown good to excellent reliability for postural control assessment in healthy adults, and the authors suggest a familiarization session as practice effects were noted before data recording [7].
All in all, this modified version of BESS allows objective measurement, that is reproducible, practical and reliable, allowing comparison to baselines and progress monitoring after training. Ideally, each athlete should have baseline data to compare before and after a concussion event, so as to safely return to competition when reaching the baseline values.
You may also like read about 12 Protocols for Balance Assessment with force/pressure plate.
>>>>Check our solutions and ask now for a quotation.
Bibliography
[1] D. R. Bell, K. M. Guskiewicz, M. A. Clark, and D. A. Padua, “Systematic review of the balance error scoring system,” Sports Health, vol. 3, no. 3, pp. 287–295, May 2011, doi: 10.1177/1941738111403122.
[2] G. L. Iverson, M. L. Kaarto, and M. S. Koehle, “Normative data for the balance error scoring system: implications for brain injury evaluations,” Brain Inj, vol. 22, no. 2, pp. 147–152, Feb. 2008, doi: 10.1080/02699050701867407.
[3] K. M. Guskiewicz, B. L. Riemann, D. H. Perrin, and L. M. Nashner, “Alternative approaches to the assessment of mild head injury in athletes,” Med Sci Sports Exerc, vol. 29, no. 7 Suppl, pp. S213-221, Jul. 1997, doi: 10.1097/00005768-199707001-00003.
[4] K. M. Guskiewicz, S. E. Ross, and S. W. Marshall, “Postural Stability and Neuropsychological Deficits After Concussion in Collegiate Athletes,” J Athl Train, vol. 36, no. 3, pp. 263–273, Sep. 2001. PMID: 12937495.
[5] C. L. Docherty, T. C. Valovich McLeod, and S. J. Shultz, “Postural control deficits in participants with functional ankle instability as measured by the balance error scoring system,” Clin J Sport Med, vol. 16, no. 3, pp. 203–208, May 2006, doi: 10.1097/00042752-200605000-00003.
[6] A. Shumway-Cook and R. Olmscheid, “A systems analysis of postural dyscontrol in traumatically brain-injured patients,” Journal of Head Trauma Rehabilitation, vol. 5, no. 4, pp. 51–62, Dec. 1990, doi: 10.1097/00001199-199012000-00007.
[7] R. M. Williams, M. A. Corvo, K. C. Lam, T. A. Williams, L. K. Gilmer, and T. C. V. McLeod, “Test-Retest Reliability and Practice Effects of the Stability Evaluation Test,” J Sport Rehabil, vol. 26, no. 3, May 2017, doi: 10.1123/jsr.2016-0163.