A Case Study - Assessment and treatment of balance dysfunction using PhysioSensing pressure plate in a patient with chronic stroke sequelae
- Ana Souto

- Sep 23, 2024
- 5 min read
Updated: Jun 13, 2025
1. Introduction
Stroke is the third leading cause of mortality and morbidity globally, with a predicted rise in prevalence creating an increased demand for rehabilitation services. Balance dysfunction, a common sequela post-stroke, significantly impairs daily activities and heightens fall risk.
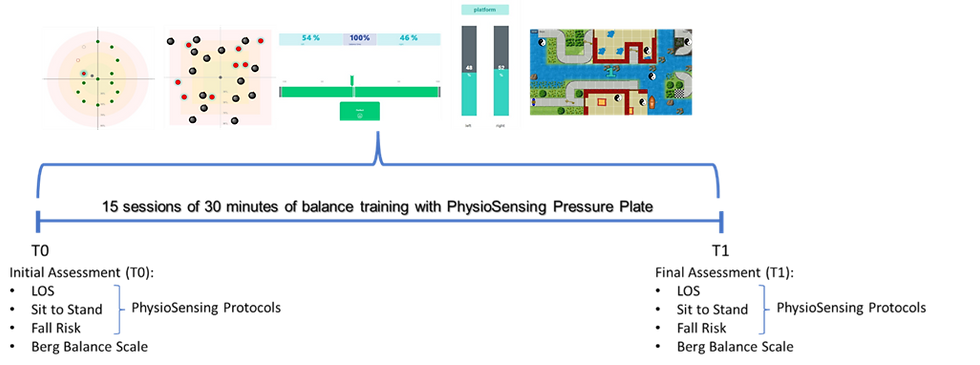
This case study investigates the impact of a 15-session balance exercise program, incorporating PhysioSensing balance plate with visual biofeedback and interactive games, on improving balance control in a 67-year-old male with chronic stroke sequelae.

2. Intervention
The intervention consisted of 15 sessions of 30 minutes of balance training performed on PhysioSensing Pressure Plate and Balance Software. Clinical and posturographic assessments were carried out before the start of the program (T0) and at the end (T1).
We decided to conduct 3 different posturography assessments. Having only a static analysis may not be enough for perceiving the reality of postural control, we need to look into how a person can maintain balance within a dynamic state, especially during functional activities. Because of this, we selected the sit-to-stand protocol and the limits of stability protocol, rather than just using the fall risk protocol.
Based on the results from the initial assessment, we chose exercises that allowed the training of 1) Weight transfers in every direction, including diagonal weight shifts, as strong correlations have been discovered between the reduced ability to voluntarily displace the center of pressure in diagonal directions and measures of balance and gait speed [1], [2], [3], 2) Direction control and the correct activation of anticipatory movement strategies [4], and 3) Symmetry of stance during sit to stand [5],[6].
2.1 Example of Exercises with PhysioSensing Pressure Plate


Exercises for training weight transfer, Limits of Stability, direction control, and the correct activation of anticipatory movement strategies, assisted with visual biofeedback.

3. Results
Sit-to-Stand Protocol

The results show clear differences in the Left/Right Symmetry where a 50% improvement can be seen. In addition, there is a marked 60% improvement on the Rising Index, meaning that the participant exerted 60% more force during the rising phase when compared with T0.
Not in the same scale as the above-referenced improvements, the results seen in Weight Time Transfer inform us that the patient was able to transfer the weight from the sited position to the beginning of the rising phase (arrival of the center of pressure over the feet) 20% faster.
To know more about how to perform and interpret the results from this protocol check the article: https://www.physiosensing.net/post/sit-to-stand-balance-protocol-how-to-use-it
Limits of Stability Protocol


Re-assessment at the end of the intervention shows a very positive impact on limits of stability, demonstrated by the increase of endpoint excursion and maximum excursion parameters, for all directions. The magnitude of the results can be seen in the percentage of improvement from T0 to T1. For the endpoint excursion, we see a one-hundred and forty % increase on average. And 90% of improvement for the maximum excursion.
Remember that a reduced area of stability is linked to a higher fall risk.

Moreover, the results also show a clear improvement in the movement velocity, accompanied by an improvement in direction control. This tells us that our intervention also impacted motor control. The participant was able to displace his center of pressure further away in all directions, significantly faster and without losing the quality of movement.
Overall, the results express enhancements in motor control, and in the ability to perform weight shifts in every direction. Daily life activities involving reaching, transfer, turning, and even gait, encompass weight shifting, therefore It is fundamental to address this in rehabilitation, especially for stroke patients where we know that it is common to see a decreased ability to do so.
To know more about how to perform and interpret the results from this protocol check the article: https://www.physiosensing.net/post/limits-of-stability-the-most-used-protocol-for-balance-assessment
Fall Risk Protocol

The results from the Fall Risk Assessment show us a shy 10% improvement. One limitation of the sway velocity index parameter is that it only considers the mediolateral sway velocity. New studies suggest that the most sensitive parameter for detecting differences between fallers and non-fallers is the sway velocity in the anteroposterior plane [7].
Compared with the results from the Sit-to-Stand Protocol and Limits of Stability, the improvement in this static assessment is more subtle. If we had only focused on static balance, we would not have found the deficits we found during sit-to-stand and the limits of stability.
To know more about how to perform and interpret the results from this protocol check the article: https://www.physiosensing.net/post/do-you-know-how-to-assess-the-fall-risk
4. Conclusion
We observed significant improvements in motor control, as reflected by increased movement velocity and enhanced directional control during the limits of stability assessment. The participant also demonstrated better weight transfer across all planes, resulting in expanded limits of stability. Furthermore, a more symmetric stance was achieved during both the rising and stabilization phases of the sit-to-stand protocol.
Do you have questions about this topic? Or want to know more about the balance system?
Schedule a 15-minute talk with me!
Ana Souto

Meet Ana, a physiotherapist with a master's degree in human physiology, currently specializing in neurobiology. Her professional journey has led her to gain extensive expertise in both neurology and sports physiotherapy.
Ana currently serves as the clinical specialist at PhysioSensing, a cutting-edge Balance Assessment and training device. Leveraging her strong foundation in scientific research and evidence-based practices, Ana creates customized assessment and training plans. Her approach is firmly rooted in the latest scientific findings, ensuring that PhysioSensing users receive the most effective and up-to-date care.
In addition to her role in designing tailored programs, Ana plays a pivotal role in guiding new clients through the learning process of using PhysioSensing. She also provides advanced training and support to existing customers seeking to further deepen their clinical practice knowledge and stay on top of the latest scientific advancements.
References
[1] M. M. Van Dijk et al., ‘A cross-sectional study comparing lateral and diagonal maximum weight shift in people with stroke and healthy controls and the correlation with balance, gait and fear of falling’, PLoS ONE, vol. 12, no. 8, p. e0183020, Aug. 2017, doi: 10.1371/journal.pone.0183020.
[2] M. Van Dijk et al., ‘Are balance and gait related to diagonal and lateral weight shifts in ambulatory people post stroke?’, Physiotherapy, vol. 102, p. e76, Nov. 2016, doi: 10.1016/j.physio.2016.10.072.
[3] K. Jung, Y. Kim, Y. Chung, and S. Hwang, ‘Weight-Shift Training Improves Trunk Control, Proprioception, and Balance in Patients with Chronic Hemiparetic Stroke’, Tohoku J. Exp. Med., vol. 232, no. 3, pp. 195–199, 2014, doi: 10.1620/tjem.232.195.
[4] S. Tasseel-Ponche, A. P. Yelnik, and I. V. Bonan, ‘Motor strategies of postural control after hemispheric stroke’, Neurophysiologie Clinique/Clinical Neurophysiology, vol. 45, no. 4–5, pp. 327–333, Nov. 2015, doi: 10.1016/j.neucli.2015.09.003.
[5] A. Brière, S. Lauzière, D. Gravel, and S. Nadeau, ‘Perception of Weight-Bearing Distribution During Sit-to-Stand Tasks in Hemiparetic and Healthy Individuals’, Stroke, vol. 41, no. 8, pp. 1704–1708, Aug. 2010, doi: 10.1161/STROKEAHA.110.589473.
[6] A. M. De Nunzio et al., ‘Biofeedback rehabilitation of posture and weight-bearing distribution in stroke: a center of foot pressure analysis’, Funct Neurol, vol. 29, no. 2, pp. 127–134, 2014.
[7] F. Quijoux et al., ‘A review of center of pressure (COP) variables to quantify standing balance in elderly people: Algorithms and open‐access code*’, Physiological Reports, vol. 9, no. 22, Nov. 2021, doi: 10.14814/phy2.15067.


